Prepare, plan and palliate – lessons learned from the ELDAC COVID-19 webinars
A guest blog post by Kim Offner, ELDAC Project Officer, Faculty of Health, University of Technology Sydney
As of May 12th, 2020, 85% of Australia’s COVID-19 deaths were in people 70 years and older, with 27% of deaths occurring in government subsidised Residential Aged Care facilities. The elderly and those with pre-existing chronic health conditions are most likely to develop serious complications of COVID-19 and have a 15-22% increased mortality rate. Rapid transmission and spread of COVID-19 through Aged Care services and facilities has been shown to occur between asymptomatic staff and residents with fatal consequences. The preparation and planning of quality symptom management and palliative care is a priority in the management of COVID-19 in the Aged Care sector.
End of Life Directions for Aged Care (ELDAC) hosted two Palliative Care COVID-19 Webinars for those working within aged care settings. The Webinars, presented in a question and answer format with expert panellists working within palliative care and aged care, aim to provide evidence-based information and guidance regarding end of life decisions in the COVID-19 context.
COVID-19 can spread through a facility before symptoms begin 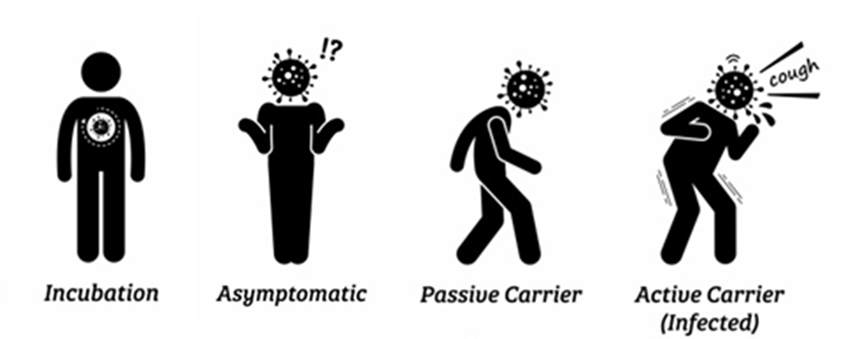
COVID-19 is transmitted via droplets, through direct contact with an infected person or following indirect contact with contaminated surfaces.
COVID-19 is highly contagious. The virus remains airborne for up to 3 hours and can survive on surfaces between 24-72 hours. Symptoms can present between 2-14 days after infection and may be very mild or non-specific. The virus, therefore, can be rapidly spread within a facility, organisation, or client base by asymptomatic carriers well before anyone presents with symptoms.
Preparation is key
 COVID-19 deterioration is rapid and can occur within hours. Preparation of palliative care resources and systems of care need to be made in advance of the first confirmed case. Consider dividing the preparation of resources into four essential components: stuff, systems, staff and space.
COVID-19 deterioration is rapid and can occur within hours. Preparation of palliative care resources and systems of care need to be made in advance of the first confirmed case. Consider dividing the preparation of resources into four essential components: stuff, systems, staff and space.
- Stuff - Organise stores of Personal Protective Equipment (PPE), end of life medications and equipment; and have these on-site. Ensure access to pulse oximetry for observation of vital signs, and oxygen. Stocks of subcutaneous cannulae, clear occlusive dressings and syringes are required to enable administration of subcutaneous medications and infusions to manage symptoms. These may be in short supply, so make provisions to use alternatives where available. Emergency COVID-19 caring@home packs and educational resources are available for the Home Care setting.
- Systems – Utilise telehealth consultations wherever possible. Clarify links to specialist palliative care services and community pharmacy providers to ensure support and supply. Identify residents and clients who do not want to be transferred to hospital, document their wishes clearly and communicate to all care providers.
- Staff –Clear and accessible protocols detailing notification, infection control and isolation are required. Develop site specific clinical management guidelines to outline staff responsibilities in the assessment, symptom control, and care of the person. Staff and care workers should practice the donning and doffing of PPE.
- Space – Identify potential areas where residents can be isolated, if required, and establish social distancing within common areas. In home care settings, quarantine appropriate space to enable handwashing, donning of PPE and storage of supplies.
Plan and deliver the best
Best practice COVID-19 management requires the proactive documentation of resident or client preferences through advance care planning. This is fundamental to person-centred palliative care that respects individual physical, psychological and spiritual needs.
A 5-7 day window exists between the commencement of COVID-19 symptoms and the development of complications, should they occur. This can enable an Advance Care Directive (ACD) to be completed for future medical treatment. An ACD can be initiated during a COVID-19 telehealth advance care planning consultation and documents completed and signed via email or fax.
Provide Palliative Care
Palliative care requires recognising a person’s pain, suffering or fear so as to provide the best possible care to alleviate distress and symptoms. In our current context we need to take a moment and consider what it means to be deteriorating with or dying from, COVID-19.
The person is likely to be breathless, confused, anxious and fearful. Most definitely though, they will be isolated and not be receiving regular visits from family or loved ones. The staff and carers they see will be wearing PPE. Our task is to provide care with compassion and empathy. Effective communication is crucial between health care staff and the person during this time, but also between staff members and with families.
Comfort care should be provided according to symptoms and include fever management, oral fluids and bed rest. Fans and nebulisers should not be used due to the likelihood of aerosolised droplet spread. Any change in health or worsening of symptoms should be assessed and current management evaluated.
Quality palliative care and symptom management is dependent on the recognition of deteriorating health and appropriate response to deterioration. Regular assessment of symptoms and vital signs will enable recognition of decline as it begins. Deteriorating health in the context of COVID-19 warrants commencement of an End of Life Care Pathway, initiation of End of Life symptom management and administration of end of life medications as required.
Conclusion
The ELDAC Webinars provide evidence-based information for aged care providers to prepare and plan the provision of palliative care during COVID-19. Decisions and preparations to access end of life medications and resources must be made well in advance of a confirmed case. Opportunities exist to initiate advance care planning to document resident or client medical treatment preferences, assess individual symptoms and enable the provision of compassionate, person-centred end of life care.

Kim Offner, ELDAC Project Officer, Faculty of Health, University of Technology Sydney