Improving serious illness conversations with families: Next steps?
An article written by Dr Nicholas Mills
The palliative care literature reports how parents value good communication with their child’s clinicians second only to pain and symptom control as a priority need. It also tells us that parents continue to advocate for the quality of serious illness communication to improve. So what might be the next steps in improving the serious illness conversations?
There is a robust research base that elucidates the perspectives and needs of children and families pertaining to serious illness communication. This has provided a foundation for the development of serious illness communication tools. However, rigid or ‘blanket’ approaches run the risk of privileging ’the uncertainty needs of health providers’ rather than the needs of patients and families. [1] We appreciate from clinical experience that a family’s cognitive and affective needs as well as their preparedness to receive information varies from day to day. A rigid approach is unlikely to be able to accommodate for this.
In our recently published work, analysis indicated that conceptualising serious illness communication as a two-step process may be important (Figure 1.). Firstly, laying the foundation for quality communication and secondly, delivering information in an effective manner.
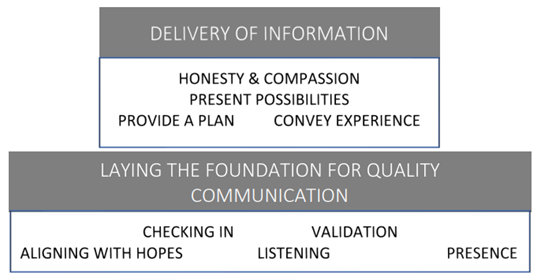
Figure 1. Approach to serious illness communication represented diagrammatically. [2]
Parents indicated that they needed to feel listened to and ‘heard’. They identified that clinicians should be routinely ‘checking-in’ as to what their needs might be before proceeding with any pre-determined agenda. Note too that, ultimately, parents looked for clinicians to convey their experience and provide a plan.
If a stable foundation for communication does not exist, clinicians may well find themselves in conflict with a family. A common example is when families do not feel listened to. Conflict is not something we are routinely taught to recognise nor manage yet the consequences are likely familiar to us. In moderate conflict, sides becomes entrenched in their views and in serious conflict communication breakdown ensues. [3]
Perhaps a next step is to develop our own skills in identifying and managing conflict quickly. Laying the foundation for quality communication by actively listening, checking-in, aligning with hopes, validating the parental experience and offering continued presence may prevent conflict or even disarm it. ‘Exploring’ rather than ’explaining’ is likely to serve clinicians well – certainly worth proceeding in that order. [3]
Author

Dr Nicholas Mills
General Paediatrician, Palliative Care Physician
Women's and Children's Hospital, Adelaide
References
- Hines SC. Coping with uncertainties in advance care planning. J Commun. 2001 Sep 1;51(3):498-513.
- Mills N, Chapman M, Sutherland I, Gillam L, Collins A. Parental perspectives on the clinician's approach to serious illness communication: A qualitative study. Palliat Support Care. 2023 Aug 1:1-6.
- Barclay S. Recognizing and managing conflict between patients, parents and health professionals. Paediatr Child Health. 2016 Jul 1;26(7):314-315.