What does a best practice model of integrated palliative care for people with advanced dementia look like translated into practice?
An article written by Dr. Suzanne Lewis
In 2019 the Central Coast Local Health District (CCLHD) began a research project to support the development of a long-term strategy for palliative and end-of-life care for the Central Coast. The research was supported by Medical Research Future Fund (MRFF) Rapid Applied Translation Grant funding through NSW Regional Health Partners. One component of the research was a rapid review of the literature to identify models of integrated palliative care for people with advanced dementia.
What does a best practice model of integrated palliative care for people with advanced dementia look like? In theory, the elements of such a model are well known. In 2014 the European Association for Palliative Care (EAPC) published a white paper defining optimal palliative care for people with dementia and in its 2022 review of standards for palliative care in Europe the Association included dementia palliative care as a specialty area. [1,2]
What does a best practice model of integrated palliative care for people with advanced dementia look like translated into practice? This question is less easily answered and is the focus of our recent review. [3] We sought examples of models that had been implemented, ideally were currently operating, and had been evaluated. Twelve dementia-specific models of end-of-life care were identified across settings in Australia, the United Kingdom, the United States, and Singapore. All the included models were complex multi-component interventions comprising health and social care services. We adapted the EAPC’s eleven domains of optimal palliative care for people with dementia and created a schema of nine domains against which we mapped the models of care we identified:
- Person-centred care
- Family care, grief, and support
- Continuity, coordination, and integration of care
- Interdisciplinary collaboration and communication
- Education
- Symptom and comfort care
- Prognostication, death, and dying
- Psychosocial and spiritual support
- Ethical and practical issues
Nine of the twelve models of care included at least some evidence of all nine domains.
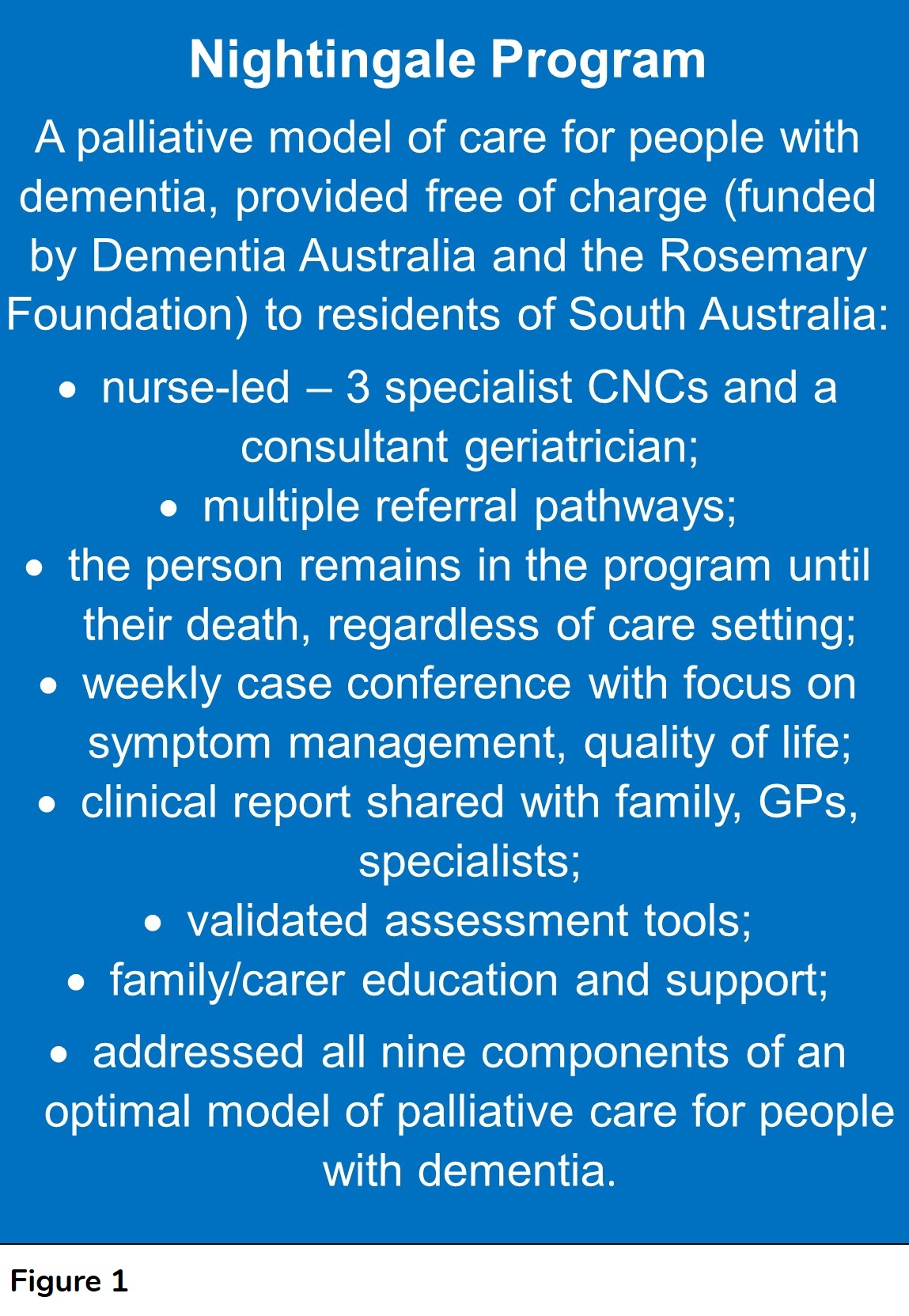 Overall, we did not find one single model with strong evidence of all the best practice components that we could take in its entirety and implement at CCLHD. The most complete and transferable model of care was the Nightingale Program (refer to Figure 1) but we could not find evidence that it had been evaluated beyond a single case study.
Overall, we did not find one single model with strong evidence of all the best practice components that we could take in its entirety and implement at CCLHD. The most complete and transferable model of care was the Nightingale Program (refer to Figure 1) but we could not find evidence that it had been evaluated beyond a single case study.
The factors essential for the successful translation of a palliative model of care for people with dementia into practice were: demonstrated best practice; ongoing funding, particularly for a dedicated care coordinator role; collaboration within and across sectors; family and carer involvement; and healthcare professional training and support (particularly in those models implemented in residential aged care). All the models of care had elements of care integration (such as a care coordination role, interdisciplinary collaboration, and person-centred care), but the level of integration varied considerably.
We envisage this rapid review will inform health managers and providers seeking an integrated approach to providing palliative care (both specialist palliative care and palliative approaches to care more generally) to people with advanced dementia who have different support needs at end of life compared to people with other life-limiting illnesses. Within this, we have provided detailed tables outlining: key components of each model of care; evaluation methods and results for those models that were evaluated; and practical examples of how domains of care were demonstrated in each of the models. There is also an extensive reference list and we note models of care still under development that are worth monitoring.
References
- van der Steen JT, Radbruch L, Hertogh CM, de Boer ME, Hughes JC, Larkin P et al. White paper defining optimal palliative care in older people with dementia: a Delphi study and recommendations from the European Association for Palliative Care. Palliat Med. 2014 Mar;28(3):197-209. doi: 10.1177/0269216313493685. Epub 2013 Jul 4.
- Payne S, Harding A, Williams T, Ling J, Ostgathe C. Revised recommendations on standards and norms for palliative care in Europe from the European Association for Palliative Care (EAPC): A Delphi study. Palliat Med. 2022 Apr;36(4):680-697. doi: 10.1177/02692163221074547. Epub 2022 Feb 3.
- Lewis S, Triandafilidis Z, Curryer C, Jeong SY, Goodwin N, Carr S et al. Models of care for people with dementia approaching end of life: A rapid review. Palliat Med. 2023 May 7:2692163231171181. doi: 10.1177/02692163231171181. Epub ahead of print.

Dr. Suzanne Lewis
Affiliate
The University of Newcastle and Library Manager
Central Coast Local Health District