Improving Patient Outcomes in Palliative Care through Point-of-Care Assessment and Benchmarking
A blog post written by Karen Quinsey, PCOC National Director
Who are we?
The Palliative Care Outcomes Collaboration (PCOC) is a nationally funded program that uses standardised clinical assessment tools to benchmark and measure patient outcomes in palliative care.
- PCOC is a collaboration between four universities, each represented by a chief investigator:
- Professor Kathy Eagar, University of Wollongong, New South Wales
- Professor David Currow, Flinders University, South Australia
- Professor Patsy Yates, Queensland University of Technology
- Dr Claire Johnson, University of Western Australia
What do we do?
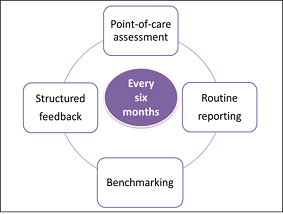
Figure 1: The PCOC Process
The program facilitates palliative care service providers to
improve patient outcomes and practice, by capturing clinically meaningful information across a patient’s disease trajectory. PCOC operates around a six month process (see Figure 1).
Five clinical assessment tools are routinely completed by participating services in hospitals and in the community. The clinical assessments are entered into a database by the palliative care service, who extract and submit the
data to PCOC (in January and July each year). A report, including nationally agreed outcome measures and benchmarks, is generated and returned to the service. Structured feedback is provided by Quality Improvement Facilitators who assist services to develop quality improvement initiatives, with the ultimate aim of improving patient outcomes.
What are PCOC reports?
The PCOC program commenced with eight palliative care services in 2006, and has since grown to include over 115 services submitting data and receiving reports. We also produce national and state level reports for each reporting cycle. The purpose of these reports is to provide the broader context of patient outcomes for palliative care in Australia. These reports are presented to national and state level organisations, for example peak bodies and Government departments.
In March 2016 the state and national reports were redesigned to better meet the needs of the readers. Following distribution of the new design of reports, 151 recipients were surveyed with 87% of respondents indicating they liked the overall look of the new format and found it easy to read, understand and use. Follow this link to see the latest national report in the new format.
What are benchmarking workshops?
A unique feature of the PCOC program is the national benchmarking workshops. Commencing in 2007, these workshops bring participating palliative care services together on an annual basis to discuss, share and understand ways to improve patient outcomes and service delivery. They also provide an opportunity for services to feedback their activities and challenges.
The most recent benchmarking workshops in June/ July brought 61 community services together to present, share and discuss benchmark information. A summary of this benchmarking workshop is available here.
What is the PCOC toolkit?
We have developed a new toolkit to support palliative care services and clinicians to implement and embed the PCOC program within the routine practice of their service. The toolkit is located here and includes the following:
- Protocol Package - includes a Guide to Implementing and Embedding PCOC, Assessment Protocol, Quality Improvement Audits and a Clinical Manual.
- Assessment Package – includes PCOC Assessment Protocol, Clinical Assessment Tools, Multilingual Symptom Assessment Scale, PCOC Assessment Forms and an Orientation to Assessment Tool.
- Mapping to National Standards – Endorsed by the Australian Commission on Safety and Quality in Health Care (ACSQHC), this resource supports the accreditation efforts of palliative care services participating in PCOC.
- Quality Improvement Audit Package – includes tools to support palliative care services to monitor and evaluate clinical assessment practice and identify areas for improvement.
Figure 2: Toolkit for Services on the PCOC Website